Suicide Prevention
Death by suicide is now, in many countries, a leading cause of death for working age adults. This is partly because of improvements in road safety and treatments for other illness - especially infections and cancers in younger people. However, it still carries a sense of stigma and uncertainty that make it somehow different to other ways of dying.
And it causes great anxiety...
The prevention of suicide is something that carries great emotion - with some saying that 100% are preventable - despite the fact that over half of people who die this way have no recent mental health contacts. We can also tend to micro-manage the more obviously risky cases, and not take a wider approach.
So perhaps we need to think more broadly...
New Zealand, where I used to live, has just published a suicide prevention strategy. Some have criticised it with being too broad, but actually I think they have it right. Prevention needs to start at the level of the population and not the individual. You don't reduce lung cancer by shouting 'stop smoking' at the person on chemotherapy who has smoked for 60 years. What are the things we can do as a society to reduce suicide overall?
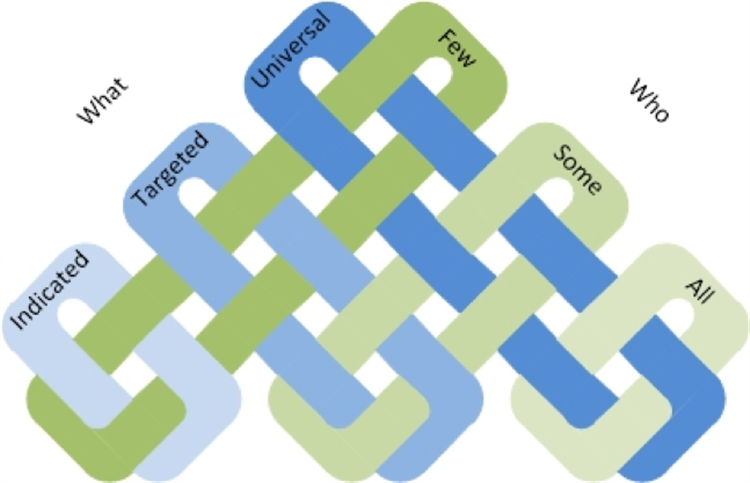
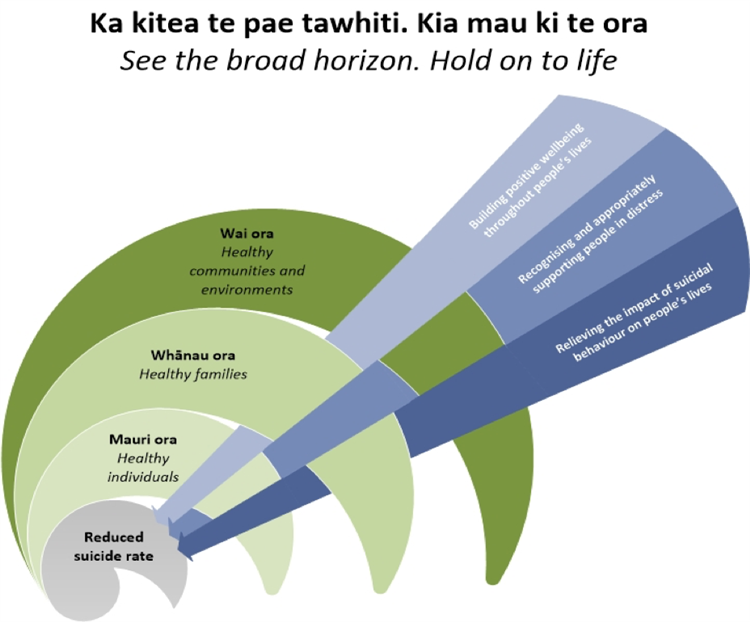
The strategy contains the graphics below which emphasise both the multiple ways we can intervene, and the cumulative effect this has. We need to act at a number of levels to affect different numbers of people:
And we need to continue to focus outwards on mental HEALTH (and wholeness) in order to impact the darker core. If we can all improve our mental health by 5%, suicide will reduce by much more because the whole pyramid has shifted down.
Some things that this might look like (from the strategy) are:
-
Education
-
Family and whanau support
-
Health and social services
-
Housing
-
Income support
-
Promoting [cultural] development
-
Mental health and wellbeing
-
Public health
-
Workplace health and safety
-
Disability issues
-
Promoting youth development
-
Employment and skills development
-
Alcohol and other drug use
-
Crime and reoffending
-
Family and sexual violence
-
Stigma and discrimination
-
Child abuse and neglect
If we can get these right, suicide will reduce.
But what about those who seem risky?
The strategy mentioned above looks at the big picture, but sometimes we will meet someone who is more specifically at risk in that moment.
The first sort of response - especially from a church or community organisation perspective - is that we should always err on the side of caution and get people to seek help. For example, we could support them to attend their GP, or it may (in the most extreme cases) look like calling an ambulance or even the police. These professionals should take this seriously if this is a new thing for this person and they are not normally suicidal.
However, sometimes mental health services will react in a different way - for example, not admitting someone to hospital who we may think is very risky. They should only do this if they know the person very well and know them to be chronically at risk and that admissions do not help.
Summary
Losing someone to suicide is a terrible thing, and we need to make seeking help easy. But we also need to focus on things that improve mental health overall and this is a real place that churches can help.
Rob Waller, 09/09/2021